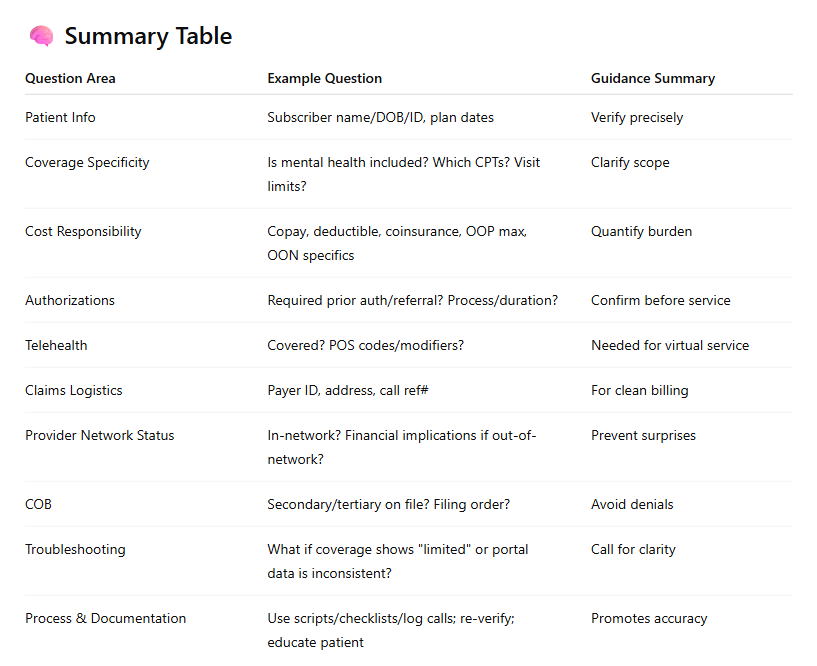
Common Questions about Eligibility Checks at Mental Health Practices
In today’s U.S. healthcare environment, billing and front office teams at mental health practices play a critical role that goes far beyond submitting claims. They are the first line of defense in ensuring that services are covered, costs are transparent, and claims are not denied for avoidable reasons. A central part of this responsibility is eligibility and benefits verification — confirming whether the patient’s insurance plan covers mental health services, and what the patient is expected to pay.
Mental health billing presents unique challenges:
- Behavioral health benefits are often "carved out" and managed by third-party administrators like Optum or Magellan, not the primary medical plan.
- Coverage is highly variable—it differs by payer, plan type, state, and employer group. Coverage for therapy, psychiatry, telehealth, and intensive outpatient programs (IOP) can vary significantly. For example, some plans may deny longer sessions like CPT 90837 (60-minute therapy) but approve shorter ones like 90834. Additionally, telehealth and IOP services are often reimbursed differently than in-person visits.
- Financial responsibility differs widely depending on in-network vs. out-of-network status and whether the patient has met their deductible or not.
A single oversight — like missing a visit limit or not confirming authorization requirements — can delay or deny payment, burden the patient with unexpected costs, and erode trust in your practice.
This guide is designed to help billing staff and front-office coordinators at mental health clinics verify benefits thoroughly and confidently. For each essential question, we've included technical guidance and real examples drawn from the field.
1. Confirming Subscriber and Policy Details
Question:
“Can you confirm the subscriber’s name, date of birth, member ID, and group number?”
Why It Matters:
Patient demographics must match exactly with payer records. Even a small discrepancy can cause electronic eligibility checks or claims to fail.
How to Verify:
- Ask the patient to provide their insurance card and confirm whether they are the primary subscriber or a dependent.
- Use payer portals or clearinghouses to validate eligibility.
- If calling, provide the patient’s full name, DOB, and member ID.
Example:
A dependent patient provides their mother’s insurance card. When verifying eligibility, use the mother’s DOB as the subscriber, not the patient’s.
2. Active Coverage and Plan Type
Question:
“Is the policy currently active? What is the effective date and termination date?”
Why It Matters:
Mental health claims are almost always denied if sessions are rendered during a period of inactive or lapsed coverage. Verifying active coverage is essential, as even minor gaps—such as a missed premium payment or a lapse in COBRA—can lead to denials.
Payers typically check effective and termination dates first when processing claims, making it crucial to confirm that coverage is active before providing care.
How to Verify:
- Check both the effective date and any termination or suspension.
- Ask if the plan is employer-sponsored, COBRA, Marketplace, or Medicaid/Medicare.
- Confirm that mental health benefits are still included under this coverage tier.
Example:
A patient with COBRA coverage may appear active in your EHR; however, the plan could have terminated (e.g., two weeks ago). If eligibility is not re-verified, claims may be submitted for inactive coverage and ultimately denied.
3. Mental Health Benefit Inclusion and Carve-Out Status
Questions:
- “Are outpatient mental/behavioral health services covered under this policy?”
- “Are these benefits managed by a third-party like Optum, Beacon, or Magellan?”
Why It Matters:
Even if a plan is active, it may not include behavioral health, or it may be administered by a separate payer.
How to Verify:
- Ask explicitly about outpatient therapy and psychiatry coverage.
- Request the name, payer ID, and contact number of any third-party behavioral health administrator.
- Determine if claims should be submitted to the primary payer or carve-out.
Example:
A patient has Aetna medical coverage, but mental health is administered by Optum. Sending claims to Aetna will result in repeated denials unless this is identified upfront.
4. CPT Code-Specific Coverage
Question:
“Are the following CPT codes covered: 90791, 90834, 90837, 99214?”
Why It Matters:
Some payers consider longer therapy sessions (like 90837) not medically necessary, or restrict psychiatry codes without a confirmed diagnosis.
How to Verify:
- Confirm coverage of each code used in your practice, especially 90837 and 99214 with add-on psychotherapy.
Front-office/billing teams must ask about specific CPT coverage during eligibility checks. This is critical because some plans exclude longer sessions (90837) or place limits on psychotherapy combined with E/M (99214 + add-on psychotherapy codes like 90833).
- Ask about documentation requirements or limitations (e.g., only a certain number of 90837 sessions per year).
Example:
For Blue Cross Blue Shield, 90834 (45-minute therapy) is always covered, but 90837 (60 minutes) requires documentation of complex trauma or dual diagnosis to be considered medically necessary.
5. Session or Visit Limits
Question:
“How many outpatients mental health visits are covered per year, and how many have been used?”
Why It Matters:
Plans often limit therapy to a fixed number of sessions per calendar or policy year.
How to Verify:
- Ask about visit caps and whether the limit applies per provider, group, or condition.
- Check if additional sessions can be authorized upon medical necessity review.
Example:
The plan covers 20 outpatient therapy visits annually. The patient has already used 18 with another provider. Your clinic can only bill for two sessions unless a prior authorization for more is approved.
6. Patient Financial Responsibility
Questions:
- ''Is the provider in-network or out-of-network for the patient’s plan?''
- “What is the specialist office copay?”
- “What is the patient’s remaining deductible?”
- “What coinsurance applies after the deductible?”
- “What is the total out-of-pocket maximum and how much is already met?”
Why It Matters:
Accurate cost estimation builds patient trust and reduces payment disputes.
How to Verify:
- Ask for exact dollar amounts — remaining deductible, met OOP maximum, applicable copay.
- Clarify if mental health visits fall under "specialist" tier.
- Confirm how cost-sharing is applied during the deductible period (e.g., is the full allowed amount patient responsibility?).
- Use a checklist or intake form to standardize the verification process. Alternatively, you can use tools like Aarogram's SmartVerify to automate verification processes.
Note: Documenting the insurance representative’s name, date, and reference number can help prevent future disputes.
Example:
The patient has a $2,000 deductible, of which $1,800 remains. After meeting the deductible, the plan pays 80%, and the patient is responsible for 20% coinsurance. Your front desk should collect the full allowed amount until the deductible is met.
Optional: Once deductible is met, switch to collecting coinsurance plus any applicable copay.
7. Prior Authorization and PCP Referral
Questions:
- “Is prior authorization required for outpatient therapy or psychiatry?”
Mention if it is an initial evaluation or an ongoing treatment — some plans only require auth for follow-ups.
- “Is a referral from the PCP required?”
Why It Matters:
Many payers require pre-approval or referrals, especially for psychiatry or when more than a limited number of sessions are needed.
How to Verify:
- Ask which CPT codes require prior authorization or referral — don’t assume it’s only for psychiatry.
- Confirm whether the PCP referral must come through a specific system (e.g., HMO portal, faxed form)
- Determine how long the authorization is valid and how many visits it covers.
- Ask for the submission method and turnaround time.
Encourage documenting any auth/referral ID number and validity period in the chart.
Example:
Cigna requires a prior auth for 99214 (psychiatry med management) if the patient sees a psychiatrist for more than 5 sessions in a 30-day window. Failure to obtain this will result in full denial.
8. Telehealth Coverage
Questions:
- “Is telehealth covered for outpatient behavioral health?”
- “Are GT or 95 modifiers required?”
Why It Matters:
Telehealth mental health services may be covered differently than in-person care, especially post-pandemic.
How to Verify:
- Ask whether telehealth from the patient’s home is allowed.
- Confirm required coding conventions — POS and modifier. Confirm whether POS 02 – Telehealth (other than home), or POS 10 – Telehealth (originating from the patient’s home)— this may vary by plan and service type.
- “Are GT or 95 modifiers required?”
- “Check if coverage is temporary (e.g., due to COVID waivers) or permanent.
- Mention phone-only visits (audio)- “Ask if audio-only sessions are covered and what codes/modifiers should be used.”
Example:
For UnitedHealthcare, telehealth is covered only when billed with POS 10 (home) and modifier 95. Claims without this modifier are denied as incomplete.
9. In-Network Status and Claims Details
Questions:
- “Is Dr. Jane Smith (NPI: 1234567890) in-network for this plan?”
- “What is the payer ID and mailing address for claims?”
Why It Matters:
Patients incur significantly higher costs when seeing out-of-network providers — and many payers don’t cover these at all.
How to Verify:
- Ask specifically about the provider’s name and NPI.
- Verify both individual and group/facility in-network status. Verify both the individual provider and group NPI — mismatched NPIs can trigger out-of-network denials.
- Request EDI payer ID and physical address for paper submissions.
- “Ask if electronic or paper claim submission is preferred and confirm any payer-specific clearinghouse requirements.”
Example:
Though your group is in-network, the individual provider is not credentialed. Claims submitted under that NPI will process as out-of-network, increasing patient cost-share dramatically.
10. Coordination of Benefits (COB)
Questions:
- “Is there a secondary or tertiary policy on file?”
- “What is the correct order of primary and secondary payers?”
Why It Matters:
Incorrect COB leads to denials or payment delays.
How to Verify:
- Confirm if the patient has additional coverage (e.g., Medicaid, commercial, or Medicare).
- Determine which policy pays first.
- If COB isn’t updated, encourage the patient to call their payer directly — practices often can’t fix this from their side.
Make a note in the patient's file if COB issues are unresolved at the time of service.
Example:
A patient has Medicare as primary and BCBS as secondary. If the COB isn’t updated, BCBS may reject claims saying Medicare should have paid first.
11. Documentation Best Practices
Why It Matters:
Thorough documentation protects your practice from denials and audit issues.
Best Practices:
- Record the name of the representative you spoke with.
- Ask for a call reference number and time of call.
- Store notes in the patient’s chart or eligibility verification system.
- Save any portal screenshots or auth approval PDFs in a patient’s billing folder or insurance tab.
Streamlining Eligibility Checks Through Automation: How Aarogram Helps
Manual eligibility verification — whether through phone calls, portal logins, or payer spreadsheets — is time-consuming, error-prone, and highly dependent on staff availability. As mental health practices grow, automation becomes essential for scaling front-office operations without sacrificing accuracy or patient experience.
Aarogram’s SmartVerify platform is designed to simplify the most repetitive and time-consuming part of front-end RCM — eligibility and benefits checks — through a combination of AI, payer integrations, and trained virtual assistants.
Here’s what it enables your billing team to do:
1. Automated Pre-Check Workflows
SmartVerify automatically runs eligibility checks 24 to 72 hours before scheduled appointments. This ensures that any issues — inactive plans, missing authorizations, or conflicting COB details — can be flagged and resolved in advance.
2. Behavioral Health-Specific Logic
Mental health plans often involve carve-outs or require checking both the medical and behavioral health payers. Aarogram’s automation logic is trained to:
- Identify when mental health benefits are managed by vendors like Optum, Magellan, Beacon, or ComPsych.
- Pull relevant details including visit limits, CPT coverage (90837, 99214, etc.), and modifier requirements for telehealth.
3. AI-Powered Benefits Interpretation
Rather than dumping raw EDI data or portal screenshots, Aarogram extracts and summarizes key financial details such as:
- Copays and coinsurance amounts
- Deductible remaining
- Authorization flags
- OON coverage risks
Your staff receives an easy-to-read, standardized summary — reducing interpretation errors and onboarding time for new team members.
4. Human-Assisted Escalations
For cases where payer data is incomplete, SmartVerify routes the check to trained assistants who will call the payer directly and fill in the missing details — including session counts, auth requirements, and rep names with call reference numbers.
Ready to Stop Chasing Insurance Details? 👉 Schedule a 15-minute demo or email us at hello@aarogram.com.